Blocked Fallopian Tubes? Causes, Symptoms, and Natural Supplement Solution
The Hidden Barrier to Motherhood
For countless women dreaming of motherhood, blocked fallopian tubes represent an invisible yet formidable obstacle. These delicate structures, each no wider than a strand of spaghetti, play an absolutely critical role in conception—serving as the pathway where sperm meets egg and where early embryonic development begins before implantation in the uterus.
Tubal factor infertility, caused by damaged or blocked fallopian tubes, accounts for approximately 25-30% of all female infertility cases, affecting millions of women worldwide. The condition often develops silently, with many women discovering the problem only after months or years of unsuccessful attempts to conceive.
What makes blocked fallopian tubes particularly challenging is their often asymptomatic nature—many women experience no obvious signs until they struggle with fertility. However, certain symptoms, risk factors, and underlying conditions can signal potential tubal issues. More importantly, while blocked tubes present significant challenges, they don't necessarily mean the end of the fertility journey.
This comprehensive guide explores the causes, symptoms, and diagnosis of blocked fallopian tubes, and examines natural supplement solutions and lifestyle approaches that may support tubal health, reduce inflammation, and optimize reproductive function. While natural approaches cannot always reverse complete blockages, they offer valuable support for overall reproductive wellness and may benefit women with partial blockages or those seeking to prevent tubal damage.
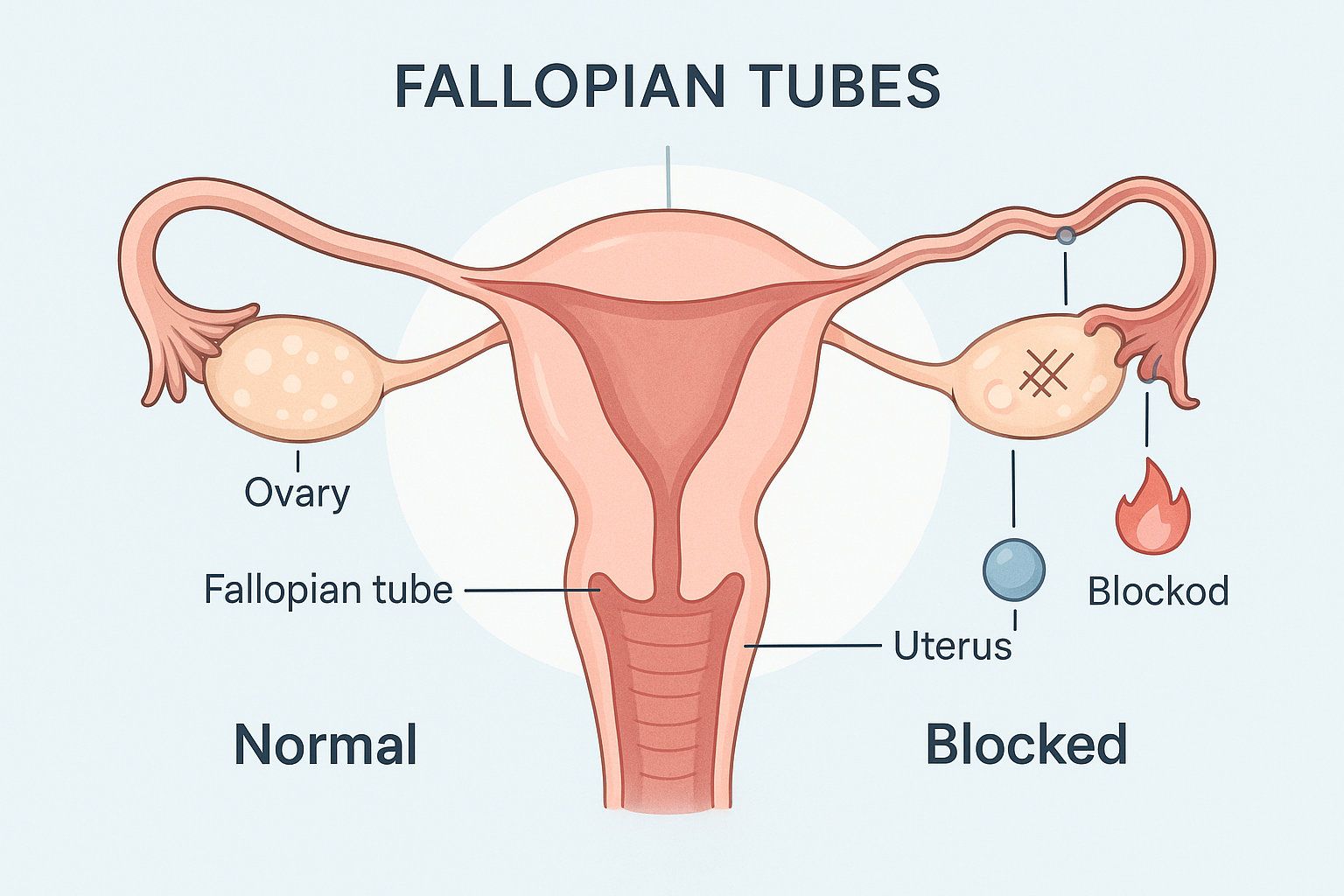
Understanding the Fallopian Tubes and Their Role in Fertility
Before exploring blockages, it's essential to understand these remarkable structures and their fertility functions.
The fallopian tubes, also called uterine tubes or oviducts, are paired organs extending from each side of the uterus toward the ovaries. Each tube measures approximately 10-12 centimeters long and consists of several segments with distinct functions:
The Fimbriae: Finger-like projections at the tube's end that sweep over the ovary surface, capturing the released egg during ovulation. These delicate structures require mobility and proper positioning.
The Ampulla: The widest portion of the tube where fertilization typically occurs. Sperm travel through the uterus and tube to reach this location, while the egg moves down from the ovary.
The Isthmus: The narrow segment connecting to the uterus, where the early embryo continues developing as it travels toward the uterine cavity.
The Interstitial Portion: The segment passing through the uterine wall, connecting the tube to the uterine cavity.
For successful conception, fallopian tubes must be:
- Patent (open): Allowing sperm to ascend and the egg/embryo to descend
- Mobile: The fimbriae must move freely to capture eggs
- Functional: Tiny hair-like structures (cilia) lining the tubes must beat rhythmically to transport the egg/embryo
- Healthy: The tubes must provide appropriate environment for fertilization and early embryonic development
Any damage, blockage, or dysfunction in these structures can significantly impair fertility.
Causes of Blocked Fallopian Tubes
Understanding what causes tubal blockages helps identify risk factors and inform prevention strategies.
Pelvic Inflammatory Disease (PID)
PID represents the most common cause of blocked fallopian tubes, accounting for a significant percentage of cases. This infection of the reproductive organs typically results from sexually transmitted infections, particularly chlamydia and gonorrhea, though other bacteria can also cause PID.
The infection triggers inflammation that damages the delicate tubal lining, causing scarring and adhesions that can partially or completely block the tubes. PID often progresses silently—approximately 70% of chlamydia infections and 50% of gonorrhea infections in women cause no symptoms, allowing the infection to persist untreated and cause substantial damage.
Research published in Human Reproduction indicates that a single episode of PID causes tubal factor infertility in approximately 12% of women, with risk increasing to 25% after two episodes and over 50% after three or more episodes.
Sexually Transmitted Infections (STIs)
Even without progressing to full PID, chlamydia and gonorrhea infections can damage fallopian tubes. These infections may cause minimal symptoms—mild pelvic discomfort, unusual discharge, or no symptoms at all—while silently scarring reproductive structures.
Studies show that untreated chlamydia infection for more than one year significantly increases tubal damage risk. This underscores the importance of regular STI screening, particularly for sexually active women under 25 and those with new or multiple partners.
Endometriosis
Endometriosis, where tissue similar to the uterine lining grows outside the uterus, frequently affects the fallopian tubes and surrounding structures. Endometrial implants and the inflammation they trigger can cause adhesions that distort, bind, or block the tubes.
Research in Fertility and Sterility found that moderate to severe endometriosis affects tubal function in many cases, though mild endometriosis may not significantly impact fertility in all women.
Previous Pelvic or Abdominal Surgery
Surgeries involving the reproductive organs, appendix, or intestines can cause adhesions—bands of scar tissue connecting structures that shouldn't be connected. These adhesions may bind the fallopian tubes to other pelvic structures, preventing proper function, or may block the tubes directly.
Previous tubal surgery, ovarian cyst removal, cesarean sections, or surgeries for ectopic pregnancy all carry risk for adhesion formation affecting tubal patency.
Ectopic Pregnancy
When a fertilized embryo implants in the fallopian tube rather than the uterus, it creates an ectopic pregnancy—a medical emergency requiring immediate treatment. The pregnancy itself and the treatment (surgical or medical) can damage the affected tube, often causing complete blockage or requiring tube removal.
Women who've had one ectopic pregnancy face increased risk for future ectopic pregnancies due to damage in the remaining tube or underlying factors that caused the first ectopic.
Hydrosalpinx
This condition involves fluid accumulation in a blocked fallopian tube, causing swelling. Hydrosalpinx typically results from previous infection or inflammation that damaged the tube, causing both blockage and fluid secretion.
The fluid-filled tube not only prevents pregnancy but may actually reduce IVF success rates if present, as the fluid can leak into the uterus and interfere with embryo implantation. Research suggests that surgical removal of hydrosalpinx before IVF improves success rates.
Fibroids and Polyps
While typically affecting the uterine cavity, large fibroids or polyps located near the tubal openings (cornua) can physically block the tubes' connection to the uterus. This type of blockage is less common but can usually be addressed surgically.
Previous Abortion or Miscarriage Complications
When abortion or miscarriage results in infection (particularly if incomplete, requiring intervention), the subsequent inflammation can damage the fallopian tubes similarly to PID. Properly performed procedures carry minimal risk, but complications or infections can affect future fertility.
Genital Tuberculosis
In regions where tuberculosis is endemic, genital TB represents a significant cause of tubal factor infertility. The infection causes severe scarring and blockage, often affecting both tubes. Genital TB is rare in developed countries but should be considered in women from endemic areas presenting with tubal infertility.
Symptoms of Blocked Fallopian Tubes
The challenging aspect of blocked fallopian tubes is that they frequently cause no symptoms. Many women have completely blocked tubes without any indication until they attempt pregnancy and encounter difficulty conceiving.
However, certain symptoms may suggest tubal issues or the underlying conditions causing blockages:
Inability to Conceive
The primary symptom is infertility itself—regular unprotected intercourse for 12 months (or 6 months if over age 35) without pregnancy. While many factors can cause infertility, tubal blockage is among the most common.
Pelvic Pain
Chronic or intermittent pelvic pain may indicate endometriosis, adhesions, or hydrosalpinx—conditions associated with tubal blockage. The pain may worsen during menstruation, ovulation, or intercourse.
Pain During Intercourse
Deep pelvic pain during or after intercourse (dyspareunia) can signal endometriosis, adhesions, or pelvic inflammatory disease—all potential causes of tubal damage.
Unusual Vaginal Discharge
Abnormal vaginal discharge—particularly if yellow, green, or foul-smelling—may indicate infection that could affect the fallopian tubes. Any unusual discharge warrants medical evaluation.
Irregular or Heavy Periods
While not directly caused by blocked tubes, heavy or irregular bleeding may indicate endometriosis or fibroids—conditions that can also affect tubal function.
Pain During Menstruation
Severe menstrual pain (dysmenorrhea), particularly if worsening over time, may suggest endometriosis, which frequently affects fallopian tubes.
History of Pelvic Infections
Previous diagnosis of PID, STIs, or pelvic infections should raise awareness of potential tubal damage, even if current symptoms are absent.
Diagnosis of Blocked Fallopian Tubes
Several diagnostic procedures can evaluate tubal patency:
Hysterosalpingography (HSG)
This x-ray procedure involves injecting contrast dye through the cervix while taking x-ray images. If tubes are open, dye flows through them and spills into the pelvic cavity (visible on x-ray). If blocked, dye stops at the blockage point. HSG can identify blockage location and severity.
Interestingly, HSG itself may have therapeutic benefits—some studies suggest the procedure may "flush out" minor blockages or debris, with some women conceiving shortly after HSG.
Sonohysterography
This ultrasound-based procedure uses saline instead of contrast dye to evaluate the uterine cavity and tubal openings. While less detailed than HSG for tubal assessment, it provides good visualization of uterine abnormalities.
Laparoscopy
This surgical procedure involves inserting a camera through small abdominal incisions to directly visualize reproductive organs. Dye can be injected through the cervix to observe tubal patency under direct visualization. Laparoscopy represents the gold standard for diagnosing tubal blockages and allows simultaneous treatment of conditions like endometriosis or adhesions.
Hysterosalpingo-Contrast Sonography (HyCoSy)
This specialized ultrasound procedure uses contrast agents to assess tubal patency without radiation exposure. It's less invasive than HSG or laparoscopy but requires specialized equipment and expertise.
Natural Supplement Solutions for Tubal Health
While natural supplements cannot definitively reverse complete tubal blockages—particularly those caused by extensive scarring—they may support overall reproductive health, reduce inflammation, support immune function, and potentially benefit women with partial blockages or those at risk for tubal damage.
It's crucial to understand that natural approaches work best as complementary strategies alongside appropriate medical evaluation and treatment. They should never replace necessary medical interventions for diagnosed tubal blockages.
Serrapeptase: The Proteolytic Enzyme
Serrapeptase, an enzyme originally derived from silkworms, has garnered attention for its potential to break down fibrin—a protein involved in scar tissue and adhesion formation. Proponents suggest that serrapeptase may help reduce adhesions and fibrosis affecting the fallopian tubes.
Research on serrapeptase's effects specifically on tubal blockages is limited, but studies have examined its anti-inflammatory and fibrinolytic (scar tissue-breaking) properties in various contexts. A study in International Journal of Surgery found that serrapeptase reduced post-surgical adhesion formation in animal models.
Typical Dosing: 10-30mg taken on an empty stomach, typically 40,000-120,000 SPU (serratiopeptidase units) daily. Effects, if any, require several months of consistent use.
Considerations: Serrapeptase has blood-thinning properties, so should be avoided by those taking anticoagulants or before surgery. Discuss with healthcare providers before use.
N-Acetyl Cysteine (NAC): The Antioxidant Powerhouse
NAC, a precursor to the powerful antioxidant glutathione, demonstrates impressive anti-inflammatory and antioxidant properties. Research has specifically examined NAC for reproductive health conditions.
A study in Human Reproduction found that NAC supplementation significantly improved conception rates in women with unexplained infertility. Another study in Fertility and Sterility showed that NAC reduced adhesion formation after gynecologic surgery—suggesting potential benefits for preventing post-surgical tubal damage.
Typical Dosing: 600-1800mg daily, divided into 2-3 doses. Higher therapeutic doses should be supervised by healthcare providers.
Additional Benefits: NAC also supports liver detoxification and may improve PCOS symptoms, making it particularly valuable for women with multiple fertility challenges.
Omega-3 Fatty Acids: Anti-Inflammatory Essential Fats
Omega-3 fatty acids, particularly EPA and DHA from fish oil, demonstrate powerful anti-inflammatory effects throughout the body. Since inflammation plays a central role in tubal damage—whether from infection, endometriosis, or adhesions—omega-3s may help reduce inflammatory processes affecting reproductive organs.
Research in American Journal of Clinical Nutrition found that higher omega-3 intake was associated with reduced inflammation markers and improved reproductive hormone profiles. While no studies specifically examine omega-3s for tubal blockages, their well-established anti-inflammatory effects support overall reproductive health.
Typical Dosing: 1000-2000mg of combined EPA/DHA daily from high-quality fish oil or algae-based supplements (for vegetarians).
Additional Benefits: Omega-3s support cardiovascular health, brain function, and healthy pregnancy when conception occurs.
Vitamin E: The Reproductive Antioxidant
Vitamin E functions as a powerful antioxidant protecting cell membranes from oxidative damage. Research suggests particular importance for reproductive health, with studies showing benefits for endometrial thickness, cervical mucus quality, and overall fertility.
While direct evidence for Vitamin E reversing tubal blockages is lacking, its antioxidant and anti-inflammatory properties support the health of all reproductive tissues, potentially benefiting tubal function.
Typical Dosing: 400-800 IU daily of natural vitamin E (d-alpha-tocopherol rather than synthetic dl-alpha-tocopherol).
Considerations: Vitamin E has mild blood-thinning properties. Those on anticoagulants should consult healthcare providers about appropriate dosing.
Turmeric/Curcumin: The Anti-Inflammatory Spice
Curcumin, the active compound in turmeric, demonstrates remarkable anti-inflammatory and antioxidant properties extensively studied in various health contexts. Its ability to reduce inflammatory pathways may benefit reproductive health, particularly conditions like endometriosis that contribute to tubal damage.
Research in Phytotherapy Research found that curcumin reduced adhesion formation in animal models of pelvic adhesions. While human studies specifically addressing tubal blockages are needed, curcumin's well-established anti-inflammatory effects support overall reproductive wellness.
Typical Dosing: 500-1000mg of curcumin extract with enhanced bioavailability (look for formulations with piperine/black pepper extract or phospholipid complexes that improve absorption).
Considerations: Turmeric may have mild blood-thinning effects and can stimulate bile production, so those with gallbladder issues should use cautiously.
Vitamin D: The Reproductive Health Essential
Vitamin D receptors are present throughout the reproductive system, and research increasingly recognizes this "vitamin" (actually a hormone) as crucial for fertility. Studies have found associations between vitamin D deficiency and various reproductive conditions including endometriosis and PCOS.
Research in Human Reproduction found that adequate vitamin D levels were associated with improved IVF outcomes, suggesting its importance for reproductive function broadly. While not directly addressing tubal blockages, optimizing vitamin D supports overall reproductive health.
Typical Dosing: 1000-4000 IU daily, ideally based on blood test results showing current levels. Target blood levels of 30-50 ng/mL for optimal reproductive health.
Considerations: Vitamin D is fat-soluble and should be taken with food containing fat for optimal absorption.
Chinese Herbal Medicine: Traditional Approaches
Traditional Chinese Medicine (TCM) has long addressed reproductive health conditions, including what Western medicine diagnoses as blocked fallopian tubes. Several herbal formulas are traditionally used to "move blood," "clear dampness," and "unblock channels"—concepts that may align with reducing inflammation and improving circulation.
Research on specific Chinese herbal formulas for tubal infertility shows mixed results. A systematic review in Evidence-Based Complementary and Alternative Medicine found that some Chinese herbal medicine formulas improved pregnancy rates in women with tubal infertility compared to no treatment, though study quality varied.
Common herbs in such formulas include:
- Dan Shen (Salvia miltiorrhiza): Promotes circulation
- Hong Hua (Carthamus tinctorius): Moves blood
- Dang Gui (Angelica sinensis): Nourishes blood
- Chi Shao (Red Peony): Moves blood and reduces inflammation
Important Note: Chinese herbs should be prescribed by qualified TCM practitioners who can create individualized formulas based on your specific pattern diagnosis. Self-prescribing complex herbal formulas is not recommended.
Lifestyle Approaches Supporting Tubal Health
Beyond supplementation, certain lifestyle factors influence reproductive health and inflammation levels:
Anti-Inflammatory Diet
Emphasizing anti-inflammatory foods while minimizing pro-inflammatory ones supports overall reproductive health:
Increase: Colorful vegetables, fatty fish, berries, leafy greens, nuts, seeds, olive oil, turmeric, ginger
Minimize: Processed foods, refined sugars, trans fats, excessive red meat, alcohol
Maintain Healthy Weight
Both overweight and underweight status can impair fertility through hormonal disruptions. Achieving healthy body weight through balanced nutrition and regular activity optimizes reproductive function.
Stress Management
Chronic stress elevates cortisol and inflammatory markers while disrupting reproductive hormone balance. Incorporating stress-reduction practices—meditation, yoga, deep breathing, counseling—supports overall reproductive wellness.
Avoid Smoking and Excessive Alcohol
Smoking significantly impairs fertility through multiple mechanisms including increased oxidative stress and inflammation. Alcohol in excess also affects reproductive health. Both should be avoided when trying to conceive.
Regular STI Screening
Since many STIs cause no symptoms while silently damaging reproductive organs, regular screening for sexually active women—particularly those under 25 or with new/multiple partners—prevents tubal damage from untreated infections.
Pelvic Physical Therapy
Specialized pelvic physical therapy, including techniques like myofascial release and visceral manipulation, may help reduce pelvic adhesions and improve pelvic blood flow. While evidence is limited, some women report benefits from working with pelvic floor physical therapists specializing in fertility.
Castor Oil Packs
Traditional naturopathic practice recommends castor oil packs applied to the lower abdomen to reduce inflammation and improve circulation. While scientific evidence is limited, this gentle, non-invasive approach has minimal risks and is used by some fertility practitioners.
When Natural Approaches Aren't Enough: Medical Options
It's crucial to understand that complete tubal blockages, particularly those caused by extensive scarring, often require medical intervention:
Tubal Surgery
Laparoscopic surgery can address certain types of tubal blockages by removing adhesions, opening blocked segments, or correcting anatomical distortions. Success depends on blockage location, extent, and the condition of remaining tubal tissue.
Proximal blockages (near the uterus) sometimes respond to procedures like tubal cannulation or catheterization. Distal blockages (near the ovary) may be treated with procedures like fimbrioplasty (repairing the fimbriae) or salpingostomy (creating a new opening).
Success rates vary widely—from 20-70% depending on damage extent and blockage type. Women with both tubes completely blocked from extensive disease typically have lower surgical success rates.
In Vitro Fertilization (IVF)
IVF bypasses the fallopian tubes entirely by fertilizing eggs outside the body and transferring embryos directly to the uterus. For women with complete bilateral tubal blockages that cannot be surgically corrected, IVF often represents the most effective treatment option.
Modern IVF success rates have improved significantly, with many clinics reporting pregnancy rates of 40-50% or higher per cycle for women under 35, declining with age.
Integrating Natural and Medical Approaches
The most effective approach for many women combines natural support with appropriate medical intervention:
- Use natural supplements and lifestyle approaches to optimize overall reproductive health, reduce inflammation, and support immune function
- Pursue appropriate medical evaluation to accurately diagnose tubal status and identify underlying causes
- Consider surgical intervention for blockages amenable to repair
- Use natural approaches before and after surgery to support healing and optimize outcomes
- Consider IVF when tubal damage is extensive or surgical approaches have been unsuccessful
- Continue natural anti-inflammatory and reproductive-supporting practices throughout fertility treatment
Supporting Your Reproductive Health Journey
Discovering blocked fallopian tubes can feel devastating, but it doesn't mean the end of your fertility journey. Whether pursuing natural approaches, medical intervention, or a combination of both, numerous options exist to support your path toward motherhood.
Natural supplement solutions—including serrapeptase, NAC, omega-3s, vitamin E, curcumin, and vitamin D—offer evidence-based support for reducing inflammation, supporting immune function, and optimizing overall reproductive health. While they cannot guarantee reversal of complete blockages, they provide valuable complementary support alongside appropriate medical care.
For comprehensive women's health supplements specifically formulated to support reproductive wellness, hormonal balance, and overall fertility, explore the collection at https://matevara.com/collections/womens-health. These carefully crafted products combine traditional wisdom with modern nutritional science to support your reproductive health journey.
Remember that every woman's situation is unique. Work with qualified healthcare providers—reproductive endocrinologists, OB/GYNs specializing in infertility, naturopathic doctors, or integrative practitioners—to develop a personalized approach addressing your specific needs, diagnosis, and goals.
Your dream of motherhood deserves comprehensive support—natural, medical, and emotional. With the right combination of approaches, many women with tubal challenges successfully achieve pregnancy and build the families they've been dreaming of.
Disclaimer: The information provided in this article is for educational and informational purposes only and is not intended as medical advice, diagnosis, or treatment. Blocked fallopian tubes represent a serious medical condition requiring professional evaluation and treatment by qualified healthcare providers specializing in reproductive medicine. This article does not constitute professional medical advice and should not replace consultation with reproductive endocrinologists, OB/GYNs, fertility specialists, or other appropriate medical professionals. Natural supplements and lifestyle approaches discussed cannot reverse complete tubal blockages caused by extensive scarring or structural damage, and should be viewed as complementary approaches alongside, not replacements for, appropriate medical evaluation and treatment. Women experiencing infertility should pursue comprehensive fertility evaluation including proper diagnosis of tubal patency through appropriate imaging or surgical procedures before relying solely on natural approaches. Delaying necessary medical treatment to pursue unproven natural remedies may reduce overall fertility success, particularly for women over 35 whose fertility declines significantly with age. The effectiveness of natural supplements for blocked fallopian tubes is not conclusively established through robust clinical trials, and individual results vary dramatically based on blockage severity, underlying causes, and individual health factors. Some supplements discussed, including serrapeptase, NAC, and vitamin E, have blood-thinning properties and may interact with medications or be contraindicated before surgery—always consult healthcare providers before starting supplementation. Ectopic pregnancy represents a life-threatening emergency; any woman with blocked or damaged fallopian tubes who suspects pregnancy and experiences pelvic pain or abnormal bleeding should seek immediate medical attention. Sexually transmitted infections require prompt medical treatment with appropriate antibiotics to prevent tubal damage—natural approaches cannot treat active infections. Pelvic inflammatory disease similarly requires immediate antibiotic treatment; delayed treatment significantly increases risk of permanent tubal damage and infertility. The supplement dosages, protocols, and recommendations provided are general guidelines and may not be appropriate for all individuals—personalized guidance from qualified healthcare providers or registered dietitians specializing in fertility is essential. Pregnancy should not be attempted while taking certain supplements without medical clearance. Women who are pregnant, nursing, have underlying health conditions, take medications, or have been diagnosed with specific reproductive disorders should consult healthcare providers before implementing any supplement regimen. The statements made about supplements and natural approaches have not been evaluated by the Food and Drug Administration. Success in conceiving depends on numerous factors beyond tubal patency, including ovarian reserve, ovulation, male factor fertility, uterine health, and overall health status. Always work with qualified fertility specialists to develop comprehensive, evidence-based treatment plans tailored to your specific diagnosis, age, health status, and reproductive goals.
Share