Magnesium for Bone Health: How It Activates Vitamin D and Unlocks Calcium
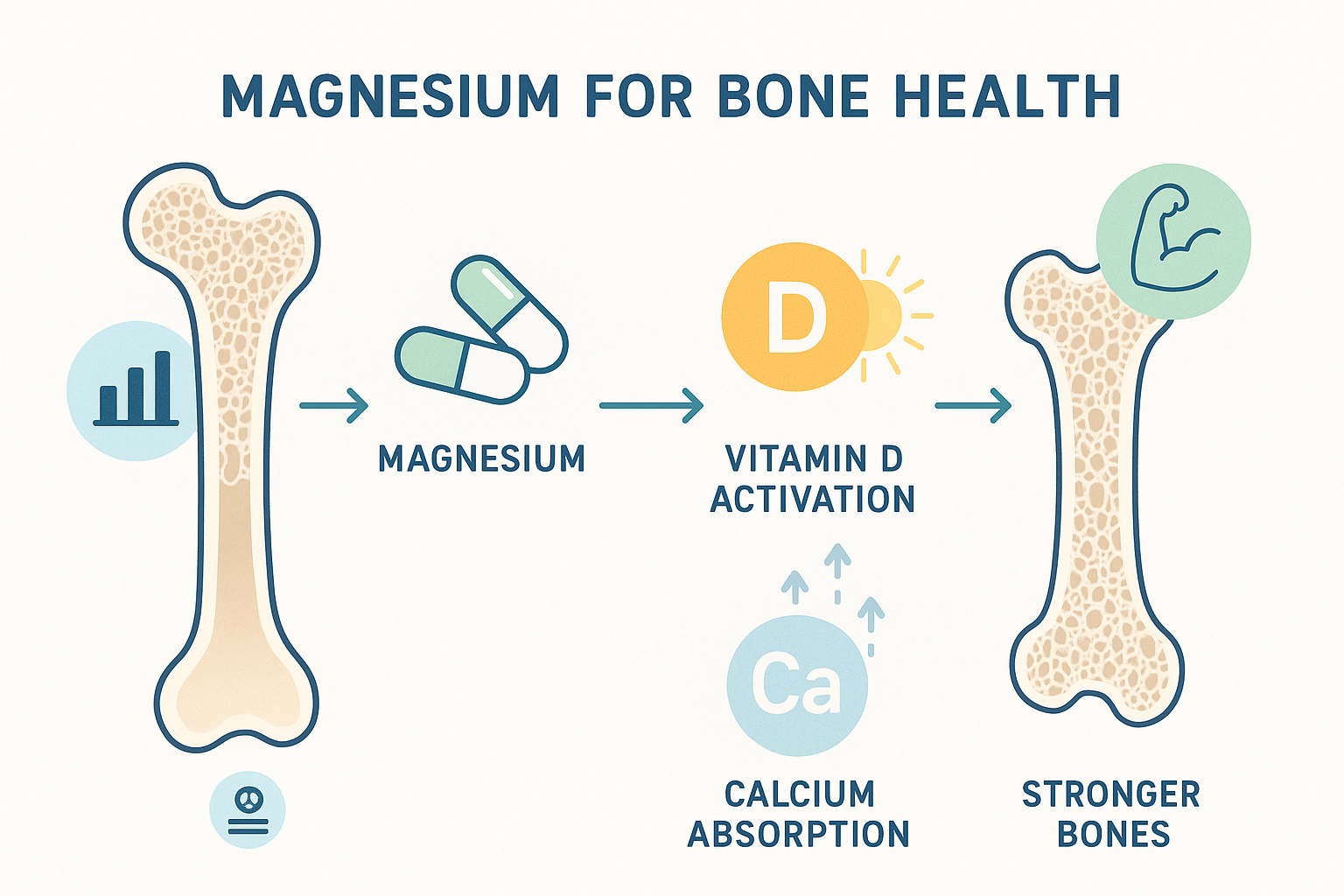
When most people think about bone health, calcium immediately comes to mind. Vitamin D usually follows close behind. But there's a third player in this bone-building trio that often gets overlooked despite being absolutely essential: magnesium. Without adequate magnesium, your calcium supplements and vitamin D might not work as effectively as you think.
Magnesium is involved in over 300 biochemical reactions in your body, and its role in bone health is both complex and critical. It doesn't just support bone density—it actually activates the vitamin D that makes calcium absorption possible and regulates where calcium gets deposited in your body. Understanding this interconnected relationship reveals why magnesium supplementation might be the missing piece in your bone health strategy.
The Hidden Epidemic: Magnesium Deficiency
Before diving into how magnesium works, it's worth understanding how common magnesium deficiency actually is. Research suggests that nearly half of Americans don't meet the recommended daily intake of magnesium through diet alone. This "hidden hunger" occurs because modern agricultural practices have depleted magnesium from soil, processed foods contain little magnesium, and certain lifestyle factors increase magnesium loss.
The consequences extend beyond bone health. Low magnesium status has been linked to cardiovascular disease, type 2 diabetes, migraines, and metabolic syndrome. But when it comes to bones specifically, magnesium deficiency can undermine your best efforts to maintain skeletal strength, even if you're taking calcium and vitamin D supplements.
The problem is that magnesium deficiency rarely causes obvious symptoms until it becomes severe. You might experience muscle cramps, fatigue, or sleep disturbances, but these signs are often dismissed or attributed to other causes. Meanwhile, your bones may be quietly suffering from the lack of this essential mineral.
Magnesium's Direct Role in Bone Structure
Approximately 60% of your body's magnesium is stored in your bones, where it serves both structural and regulatory functions. Magnesium forms part of the bone mineral crystal structure itself, contributing to bone hardness and strength. Think of it as being woven into the very fabric of your skeletal system.
At the cellular level, magnesium influences the activity of osteoblasts—the cells responsible for building new bone tissue. It also affects osteoclasts, the cells that break down old bone. This balance between bone formation and bone resorption is crucial for maintaining healthy bone throughout your life. When magnesium levels are low, this delicate balance can shift toward excessive bone breakdown.
Studies have consistently shown a positive association between magnesium intake and bone mineral density. Research published in the American Journal of Clinical Nutrition found that higher magnesium intake was associated with greater bone mineral density in both men and women. Another study in the European Journal of Epidemiology involving over 73,000 postmenopausal women found that those with the highest magnesium intake had significantly higher bone mineral density than those with the lowest intake.
But magnesium's most fascinating role in bone health isn't just about being a structural component—it's about how it activates and regulates the other key players in bone metabolism.
The Vitamin D Activation Connection
Here's where magnesium's role becomes truly essential: it's required to convert vitamin D into its active form. Without sufficient magnesium, the vitamin D you get from sun exposure, food, or supplements cannot be properly activated, rendering it largely ineffective for calcium absorption and bone health.
The process works like this: Vitamin D goes through two conversion steps to become its active form, calcitriol. The first conversion happens in the liver, and the second occurs in the kidneys. Both of these conversion steps require magnesium-dependent enzymes. Without adequate magnesium, these enzymes cannot function properly, and vitamin D remains in its inactive form.
A groundbreaking study published in the Journal of the American Osteopathic Association in 2018 found that magnesium deficiency could make vitamin D ineffective. The researchers noted that magnesium supplementation substantially reversed resistance to vitamin D treatment in people with chronic diseases. This finding has profound implications: taking high doses of vitamin D without sufficient magnesium might not provide the bone-protective benefits you're seeking.
This explains why some people take vitamin D supplements yet still show low levels of active vitamin D in blood tests. The vitamin D isn't the problem—the lack of magnesium to activate it is. It's like having a key (vitamin D) but no way to turn it in the lock (magnesium-dependent enzymes).
Unlocking Calcium: Magnesium as the Gatekeeper
The relationship between magnesium and calcium is intricate and delicate. While calcium needs to be absorbed and deposited in bones, it shouldn't end up in soft tissues where it can cause problems like arterial calcification, kidney stones, or muscle stiffness. Magnesium acts as a natural gatekeeper, regulating calcium transport and deposition.
Magnesium influences calcium metabolism in several critical ways:
Parathyroid Hormone Regulation: Magnesium is essential for the proper secretion and function of parathyroid hormone (PTH), which regulates calcium levels in your blood and bones. When magnesium is deficient, PTH secretion becomes impaired, disrupting the entire calcium regulation system. This can lead to hypocalcemia (low blood calcium) despite adequate calcium intake, because the regulatory mechanism isn't working properly.
Calcium Channel Management: At the cellular level, magnesium acts as a natural calcium channel blocker, controlling how much calcium enters cells. This prevents calcium overload in cells and tissues where excess calcium can be harmful. In bones, proper calcium channel function ensures calcium is deposited in the bone matrix rather than in surrounding soft tissues.
Calcitonin Production: Magnesium also influences calcitonin, a hormone that helps draw calcium from the blood and soft tissues into the bones. Low magnesium levels can reduce calcitonin effectiveness, meaning calcium may not be efficiently directed to where it's needed most—your skeletal system.
Research published in Nutrients journal demonstrated that the ratio of calcium to magnesium intake matters significantly for bone health. The ideal ratio appears to be around 2:1 (calcium to magnesium). Western diets often have ratios of 5:1 or higher, which may actually be counterproductive for bone health and increase the risk of cardiovascular calcification.
The Calcium Paradox: When More Isn't Better
The conventional wisdom has been to take high-dose calcium supplements for bone health. However, emerging research suggests this approach may be misguided without adequate magnesium. This phenomenon has been termed the "calcium paradox"—situations where calcium intake is high but bone health is poor, often accompanied by calcium depositing in arteries and soft tissues.
When you take calcium supplements without sufficient magnesium, several problems can occur:
The calcium may not be properly absorbed from your intestines due to insufficient activated vitamin D (which, as we've learned, requires magnesium for activation). Even if absorbed, the calcium might not be efficiently directed to your bones because the regulatory hormones (PTH and calcitonin) aren't functioning optimally without magnesium. Excess calcium that isn't deposited in bones can accumulate in soft tissues, potentially contributing to arterial calcification, kidney stones, and muscle stiffness.
A meta-analysis published in the British Medical Journal examined calcium supplementation and cardiovascular risk, finding a potential increased risk of myocardial infarction with calcium supplements. While this research remains controversial, it highlights the importance of balanced mineral intake rather than focusing on calcium alone.
The lesson here is clear: calcium doesn't work in isolation. It requires a supporting cast of nutrients, with magnesium playing a starring role.
Scientific Evidence: Magnesium and Osteoporosis Prevention
The connection between magnesium and osteoporosis has been explored in numerous studies with compelling results. Osteoporosis, characterized by decreased bone density and increased fracture risk, affects millions worldwide, particularly postmenopausal women. While calcium and vitamin D have received most of the attention, magnesium may be equally important.
The Framingham Heart Study, one of the longest-running epidemiological studies, found that higher magnesium intake was associated with higher bone mineral density in both men and women. Participants with the highest magnesium intake had significantly better bone density compared to those with the lowest intake, even after adjusting for other factors.
Clinical trials have provided even more direct evidence. A study published in Biological Trace Element Research examined postmenopausal women with osteoporosis who were given either magnesium supplements or a placebo for two years. The magnesium group showed significant increases in bone mineral density, while the control group experienced continued bone loss. The researchers concluded that magnesium supplementation could help prevent osteoporotic fractures.
Another study in the American Journal of Clinical Nutrition followed nearly 2,000 middle-aged and elderly men and women for four years. The results showed that adequate magnesium intake was protective against bone loss, particularly in the hip and spine—areas most vulnerable to osteoporotic fractures.
Research has also examined fracture risk directly. A study involving over 6,000 participants found that those with the highest dietary magnesium intake had a 27% lower risk of fractures compared to those with the lowest intake. This protective effect remained significant even after accounting for calcium and vitamin D intake.
How Much Magnesium Do You Need?
The recommended dietary allowance for magnesium varies by age and gender. Adult men need approximately 400-420 mg daily, while adult women require 310-320 mg daily. Pregnant women need slightly more, around 350-360 mg daily. These requirements increase with age, physical activity, and certain health conditions.
However, meeting these requirements through diet alone can be challenging in modern life. The best dietary sources of magnesium include:
Dark leafy greens like spinach and Swiss chard are magnesium powerhouses, providing significant amounts per serving. Nuts and seeds, particularly pumpkin seeds, almonds, and cashews, offer concentrated magnesium along with healthy fats. Whole grains contain more magnesium than refined grains, making them a better choice for overall nutrition. Legumes such as black beans, chickpeas, and lentils provide both magnesium and protein. Dark chocolate (70% cacao or higher) offers a delicious source of magnesium. Fatty fish like salmon and mackerel provide magnesium along with vitamin D and omega-3 fatty acids. Avocados offer magnesium along with healthy fats and other nutrients.
Despite these dietary sources, supplementation often becomes necessary, especially for people with increased needs or absorption issues. When considering supplementation, the form of magnesium matters significantly.
Choosing the Right Magnesium Supplement
Not all magnesium supplements are created equal. The form of magnesium affects both its absorption rate (bioavailability) and its specific effects in the body. Here are the most common forms:
Magnesium Citrate: This highly bioavailable form is well-absorbed and often recommended for general supplementation. It has a mild laxative effect at higher doses, which can be beneficial for people with constipation but may be problematic for others.
Magnesium Glycinate: Bound to the amino acid glycine, this form is gentle on the digestive system and less likely to cause loose stools. It's often recommended for people who need higher doses or have sensitive digestive systems. The glycine component may also promote relaxation and sleep.
Magnesium Threonate: This newer form can cross the blood-brain barrier and has been studied for cognitive benefits. While not specifically targeted for bone health, it provides systemic magnesium that supports overall function.
Magnesium Oxide: While inexpensive and widely available, this form has relatively poor absorption compared to other forms. Much of it passes through the digestive system without being absorbed, though it can be effective for relieving constipation.
Magnesium Malate: Bound to malic acid, this form may be particularly beneficial for people with fatigue or muscle pain. It's reasonably well-absorbed and gentle on the digestive system.
For bone health specifically, magnesium citrate and magnesium glycinate are generally considered the best choices due to their high bioavailability and tolerability. Some bone health supplements combine multiple forms to optimize both absorption and effects.
The Optimal Bone Health Stack
Understanding how magnesium, calcium, and vitamin D work together allows us to create a more effective bone health strategy. Rather than taking high-dose calcium supplements alone, consider a balanced approach:
Magnesium: 300-400 mg daily from supplements, plus dietary sources. Choose a highly bioavailable form like citrate or glycinate.
Calcium: 500-700 mg from supplements if dietary intake is insufficient, aiming for a total intake of 1,000-1,200 mg daily from all sources. Don't exceed 500 mg per dose for better absorption. Remember that many foods provide calcium, so you may not need as much supplementation as you think.
Vitamin D3: 1,000-2,000 IU daily, or as recommended based on blood test results. Some people require higher doses, particularly those living in northern climates or with limited sun exposure.
Vitamin K2: This often-overlooked nutrient works with vitamin D to direct calcium into bones rather than soft tissues. A dose of 100-200 mcg daily of MK-7 (the longer-acting form) complements the magnesium-calcium-vitamin D trio.
Trace Minerals: Boron, zinc, copper, and manganese all play supporting roles in bone health. A comprehensive bone health supplement should include these in appropriate amounts.
The timing of supplementation can also matter. Calcium and magnesium can compete for absorption, so some experts recommend taking them at different times of day. However, the evidence for this strategy is mixed, and convenience may trump optimal timing for ensuring consistent supplementation.
Who Needs Extra Magnesium for Bone Health?
While everyone needs adequate magnesium, certain groups are at higher risk for deficiency and may particularly benefit from supplementation:
Postmenopausal women face accelerated bone loss due to declining estrogen levels. Ensuring adequate magnesium intake becomes even more critical during this period. Studies show that magnesium supplementation can help slow bone loss in postmenopausal women.
Older adults generally absorb nutrients less efficiently and may have reduced dietary intake. Age-related decrease in stomach acid production can impair magnesium absorption, making supplementation more important.
People with digestive disorders such as Crohn's disease, celiac disease, or chronic diarrhea often have impaired mineral absorption. These individuals may need higher doses of easily absorbed forms of magnesium.
Athletes and highly active individuals lose magnesium through sweat and have increased needs due to higher metabolic demands. This population often focuses on calcium for bone health but may neglect magnesium.
People taking certain medications including proton pump inhibitors (for acid reflux), diuretics, and some antibiotics can experience accelerated magnesium loss or reduced absorption. If you're on these medications long-term, monitoring your magnesium status is important.
Individuals with type 2 diabetes tend to excrete more magnesium in urine and often have lower magnesium levels. This creates a double concern, as both diabetes and magnesium deficiency can affect bone health.
Those with high calcium intake from supplements or fortified foods may need additional magnesium to maintain the proper calcium-to-magnesium ratio and prevent calcium from depositing in the wrong places.
Beyond Bone Density: Magnesium's Full Impact
While this article focuses on bone health, it's worth noting that optimizing your magnesium status offers benefits far beyond your skeleton. The same magnesium that activates vitamin D and regulates calcium also:
Supports cardiovascular health by helping maintain normal blood pressure and preventing arterial calcification. Regulates blood sugar by improving insulin sensitivity and glucose metabolism. Enhances muscle function and reduces cramps by balancing calcium's contracting effect with magnesium's relaxing effect. Promotes better sleep through its calming effects on the nervous system. Reduces inflammation throughout the body. Supports healthy mood and stress response through its effects on neurotransmitters.
This means that supplementing magnesium for bone health delivers multiple benefits simultaneously. You're not just protecting your skeleton—you're supporting your entire body's function.
Recognizing Magnesium Deficiency
Since overt magnesium deficiency is relatively rare but insufficient magnesium intake is common, recognizing the subtle signs becomes important:
Muscle cramps or twitches, particularly in the legs at night, are classic signs of insufficient magnesium. Persistent fatigue or weakness that doesn't improve with rest may indicate low magnesium. Sleep difficulties, including trouble falling asleep or restless sleep, can be related to magnesium status. Abnormal heart rhythms or palpitations sometimes relate to magnesium deficiency. Frequent headaches or migraines may be more common with low magnesium levels. Anxiety or irritability can worsen when magnesium is insufficient. Loss of appetite, nausea, or vomiting can occur with more severe deficiency.
If you experience multiple these symptoms, particularly if you're also concerned about bone health, discussing magnesium supplementation with your healthcare provider makes sense. Blood tests can measure magnesium levels, though standard serum magnesium tests may not fully reflect magnesium status in tissues and bones.
Making Magnesium Work for Your Bones
Understanding the science is one thing; applying it effectively is another. Here's how to make magnesium work optimally for your bone health:
Start with diet: Before reaching for supplements, optimize your dietary magnesium intake. Build meals around magnesium-rich whole foods. This approach provides magnesium along with other beneficial nutrients and fiber.
Supplement strategically: If your diet falls short or you have increased needs, choose a high-quality, bioavailable form of magnesium. Start with moderate doses and increase gradually to avoid digestive upset.
Balance your minerals: Remember that magnesium works in concert with calcium, vitamin D, and vitamin K2. A comprehensive approach beats supplementing single nutrients in isolation.
Consider absorption enhancers: Taking magnesium with vitamin B6 may enhance absorption. Vitamin D (which magnesium activates) also improves magnesium absorption, creating a beneficial feedback loop.
Time it right: If you experience digestive upset, divide your magnesium dose throughout the day rather than taking it all at once. Some people find taking magnesium in the evening promotes better sleep as a bonus benefit.
Be consistent: Like all nutritional interventions for bone health, magnesium supplementation requires consistency over months and years to show meaningful benefits. This isn't a quick fix but a long-term investment in your skeletal strength.
Monitor your progress: If you're at risk for osteoporosis, regular bone density scans can help you track whether your nutritional approach is working. Discuss your supplementation strategy with your healthcare provider.
The Future of Bone Health: A More Complete Picture
The understanding of bone health has evolved significantly over recent decades. We've moved from viewing it as simply a calcium issue to recognizing the complex interplay of multiple nutrients, hormones, and lifestyle factors. Magnesium's role in activating vitamin D and regulating calcium represents a crucial piece of this more complete puzzle.
Emerging research continues to refine our understanding. Scientists are investigating optimal ratios of bone-supporting nutrients, the role of the gut microbiome in mineral absorption, and how inflammation affects bone metabolism. Personalized nutrition based on genetic factors may eventually allow tailored recommendations for bone health supplementation.
What remains clear is that focusing solely on calcium supplementation while neglecting magnesium is an incomplete and potentially counterproductive approach. The three-way relationship between magnesium, vitamin D, and calcium forms the foundation of an evidence-based bone health strategy.
Take Control of Your Bone Health Today
Your bones are living tissue that responds to the nutrients you provide. While genetics play a role in bone health, your nutritional choices matter enormously. Ensuring adequate magnesium intake—whether through diet, supplementation, or both—gives your body the tools it needs to activate vitamin D, regulate calcium properly, and build strong, resilient bones throughout your life.
Don't wait until a fracture or osteoporosis diagnosis forces you to pay attention to your bones. The time to support your skeletal health is now, regardless of your age. Every meal that includes magnesium-rich foods and every day of consistent supplementation contributes to a stronger, more resilient skeleton.
Ready to give your bones the comprehensive support they deserve? Explore science-backed bone and joint health supplements at Matevara's Bone & Joint Health Collection. Their carefully formulated products provide the balanced nutrition your bones need, including optimal ratios of magnesium, calcium, vitamin D, and supporting nutrients. Invest in your skeletal strength today for a more active, independent tomorrow.
Disclaimer: This article is provided for informational and educational purposes only and should not be considered medical advice or a substitute for consultation with qualified healthcare professionals. The information presented is based on current scientific research and general knowledge about magnesium and bone health, but individual needs and responses to supplementation vary significantly. Before starting any new supplement regimen, including magnesium supplementation, you should consult with your healthcare provider, particularly if you have existing medical conditions such as kidney disease, heart conditions, or digestive disorders, are taking prescription medications that may interact with magnesium, or are pregnant or nursing. Magnesium supplements can interact with various medications including antibiotics, bisphosphonates, diuretics, and proton pump inhibitors. People with impaired kidney function should exercise particular caution as excess magnesium can accumulate to dangerous levels when kidneys cannot properly excrete it. The statements regarding supplements have not been evaluated by the Food and Drug Administration, and these products are not intended to diagnose, treat, cure, or prevent any disease. Bone health outcomes depend on multiple factors including genetics, overall diet, physical activity, hormonal status, and lifestyle factors beyond supplementation alone. Always follow recommended dosages and purchase supplements from reputable sources with third-party testing to ensure quality and purity.
Share