Struggling with Muscle Pain? Discover Causes, Symptoms and Effective Solutions
Muscle pain is a universal human experience. Whether you're an athlete pushing physical limits, someone managing a chronic condition, a weekend warrior returning to exercise after time off, or simply dealing with the strains of daily life, muscle discomfort can significantly impact your wellbeing. The challenge lies in understanding why your muscles hurt and, more importantly, what you can do about it.
Muscle pain ranges from mild soreness that fades within days to chronic, debilitating discomfort that persists for months. The underlying causes are equally diverse—spanning acute injuries, overuse patterns, inflammatory conditions, nutritional deficiencies, stress responses, and systemic diseases. Without understanding the specific cause of your muscle pain, finding effective solutions becomes a frustrating trial-and-error process.
This comprehensive guide demystifies muscle pain by exploring its various origins, helping you identify different types of muscle discomfort through their distinctive symptoms, and providing actionable, evidence-based solutions that address both immediate relief and long-term prevention. By the end, you'll have a clear framework for managing muscle pain effectively while knowing when professional medical evaluation is necessary.
Understanding Muscle Pain: Types and Mechanisms
Muscle pain, medically termed myalgia, manifests through different mechanisms depending on its cause. Understanding these distinctions helps guide appropriate treatment approaches.
Acute Muscle Pain
Acute muscle pain develops suddenly, typically following a specific incident or activity. This category includes delayed onset muscle soreness (DOMS), muscle strains and tears, acute overuse injuries, and trauma-related muscle damage. Acute pain is usually self-limiting, resolving within days to weeks with appropriate care.
DOMS, the soreness that peaks 24-72 hours after unaccustomed exercise, results from microscopic damage to muscle fibers and the inflammatory response that follows. While uncomfortable, DOMS represents a normal adaptation process and actually signals that your muscles are responding to training stimulus.
Chronic Muscle Pain
Chronic muscle pain persists beyond three months and often lacks a clear triggering event. Common causes include fibromyalgia, myofascial pain syndrome, chronic tension patterns, inflammatory conditions like polymyalgia rheumatica, and metabolic myopathies. Chronic pain requires comprehensive evaluation to identify underlying causes and may need multifaceted treatment approaches.
Referred Pain
Sometimes, what feels like muscle pain actually originates elsewhere. Internal organ problems, nerve compression, joint issues, and vascular problems can all produce sensations perceived as muscle pain. This is why persistent or unusual muscle pain warrants medical evaluation to rule out serious underlying conditions.
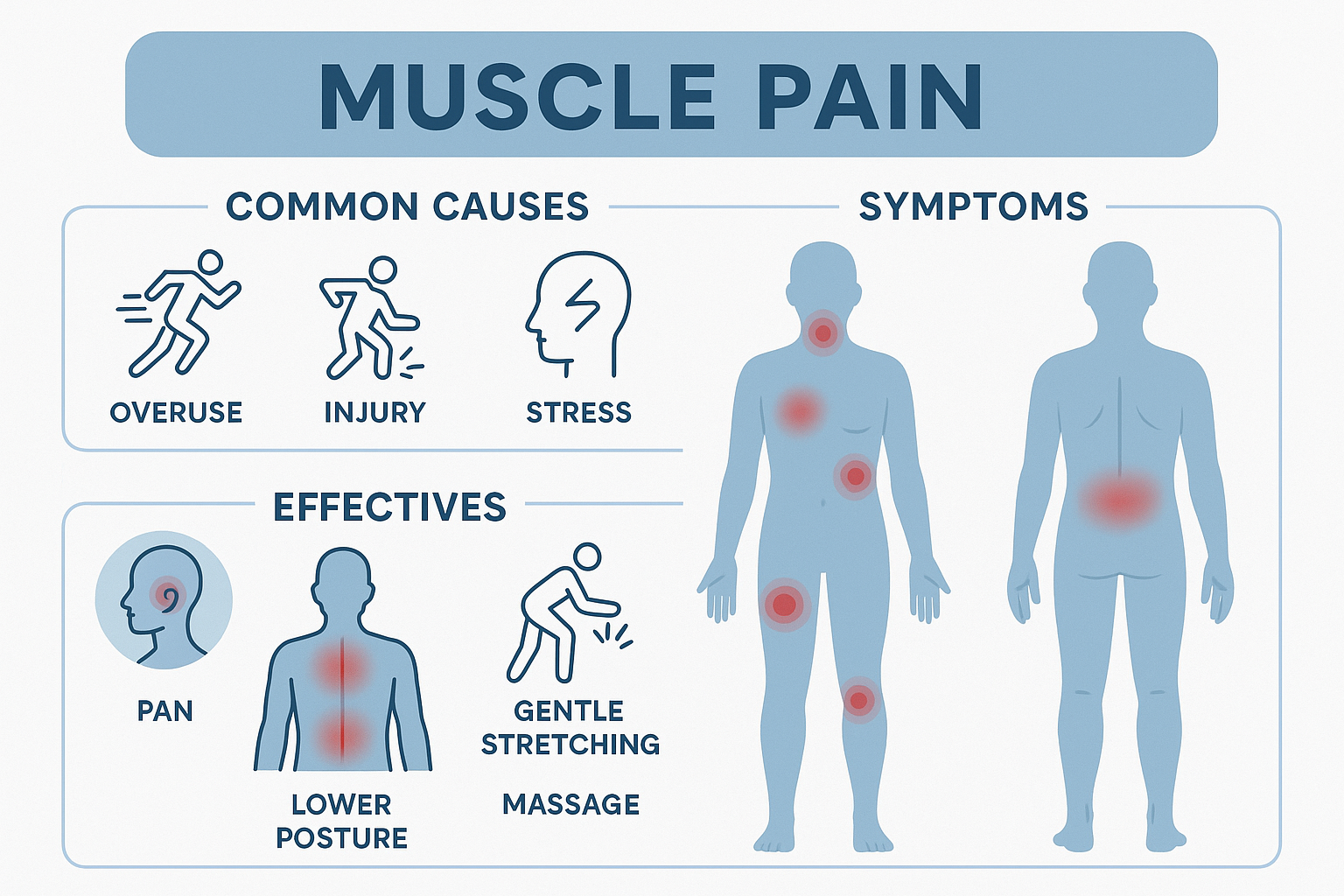
Common Causes of Muscle Pain
Identifying the cause of your muscle pain is essential for selecting effective treatments. The following represent the most frequent culprits behind muscle discomfort.
Exercise and Physical Activity
The most common cause of muscle pain is physical activity, particularly when intensity, duration, or type of exercise exceeds what your muscles are accustomed to. Eccentric contractions—where muscles lengthen under tension, such as running downhill or lowering weights—cause the most significant DOMS.
New exercise routines, increased training volume or intensity, inadequate warm-up or cool-down, and poor exercise technique all increase risk of exercise-induced muscle pain. While this type of soreness is normal and temporary, understanding how to minimize discomfort and optimize recovery improves your training experience.
Muscle Injuries
Acute injuries cause immediate and often severe muscle pain. Muscle strains occur when fibers stretch excessively or tear, ranging from mild (grade 1) to complete rupture (grade 3). Contusions result from direct impact causing bleeding within the muscle. Muscle cramps involve sudden, involuntary, painful contractions often triggered by dehydration, electrolyte imbalances, or muscle fatigue.
Overuse and Repetitive Strain
Repetitive movements without adequate recovery create cumulative microtrauma. Office workers develop neck and shoulder tension, athletes experience sport-specific overuse injuries, manual laborers suffer from chronic muscle strain, and people with poor posture develop persistent muscle pain in the back, neck, and shoulders. Overuse injuries develop gradually and worsen without intervention addressing the underlying movement pattern or workload.
Nutritional Deficiencies
Muscles require specific nutrients for proper function and recovery. Deficiencies cause weakness, cramping, and pain. Key deficiencies include vitamin D (essential for muscle function, with deficiency causing widespread pain and weakness), magnesium (critical for muscle relaxation, with deficiency causing cramps and spasms), potassium (important for muscle contraction, with low levels causing weakness and cramping), calcium (necessary for contraction-relaxation cycles), and B vitamins (supporting energy production and nerve function).
Dehydration and Electrolyte Imbalances
Adequate hydration and electrolyte balance are essential for muscle function. Dehydration reduces blood flow to muscles, impairs waste removal, increases cramping risk, and reduces performance. Electrolyte imbalances—particularly sodium, potassium, and magnesium—disrupt the electrical signals controlling muscle contraction and relaxation.
Stress and Tension
Psychological stress manifests physically through chronic muscle tension. The body's stress response triggers muscle contraction, preparing for "fight or flight." When stress becomes chronic, muscles remain in a partially contracted state, causing persistent discomfort particularly in the neck, shoulders, upper back, and jaw. This tension creates a vicious cycle where pain increases stress, which further tightens muscles.
Inflammatory Conditions
Various inflammatory conditions cause diffuse muscle pain. Viral infections like influenza and COVID-19 commonly cause myalgia. Autoimmune conditions including lupus, rheumatoid arthritis, and polymyositis attack muscle tissue. Fibromyalgia causes widespread muscle pain along with fatigue and sleep disturbances. These conditions require medical diagnosis and management.
Medications
Certain medications cause muscle pain as a side effect. Statins (cholesterol-lowering drugs) are notorious for causing myopathy in some users. Other culprits include ACE inhibitors for blood pressure, some antibiotics, and chemotherapy agents. If muscle pain develops after starting new medication, discuss it with your healthcare provider—never discontinue prescribed medications without medical guidance.
Poor Circulation
Peripheral artery disease and other circulatory problems reduce oxygen delivery to muscles, causing pain particularly during activity. This claudication pain typically occurs in the legs during walking and improves with rest. Circulation-related muscle pain requires medical evaluation and treatment of underlying vascular issues.
Recognizing Symptoms: When to Worry
Not all muscle pain is created equal. Recognizing concerning symptoms helps you determine when self-care is appropriate versus when medical evaluation is necessary.
Normal Muscle Soreness Characteristics
Typical DOMS and mild muscle fatigue present with dull, achy discomfort that's diffuse rather than localized to a specific point, peaks 24-72 hours after exercise, gradually improves over 5-7 days, doesn't prevent normal daily activities despite discomfort, and responds to gentle movement, heat, and basic self-care measures.
Warning Signs Requiring Medical Attention
Seek medical evaluation if you experience severe pain that prevents normal movement or daily activities, sudden onset of intense pain without clear cause, pain accompanied by significant swelling, redness, or warmth (suggesting possible infection), muscle weakness that persists or worsens, numbness or tingling along with muscle pain, pain that worsens progressively rather than improving, dark-colored urine (potentially indicating rhabdomyolysis, a serious condition), fever along with muscle pain, pain following injury with visible deformity, or chronic pain lasting beyond three months without improvement.
Distinguishing Muscle Pain from Other Conditions
Muscle pain differs from joint pain (which is typically localized to the joint space and worsens with movement of that specific joint), nerve pain (which often causes shooting, burning, or electric sensations along nerve pathways), bone pain (which is deep, constant, and doesn't vary much with rest or movement), and cardiac pain (which may present as chest, shoulder, or arm discomfort along with shortness of breath, nausea, or sweating).
If you're uncertain whether your pain is muscular or potentially related to more serious conditions, err on the side of caution and seek medical evaluation.
Effective Solutions for Muscle Pain Relief
Managing muscle pain effectively requires addressing both immediate symptoms and underlying causes. The following evidence-based strategies provide relief while supporting healing.
Immediate Relief Strategies
When muscle pain strikes, several approaches provide quick relief. The RICE protocol (Rest, Ice, Compression, Elevation) remains effective for acute injuries, particularly within the first 48-72 hours. Rest the affected muscle to prevent further damage. Ice reduces inflammation and numbs pain—apply for 15-20 minutes every 2-3 hours. Compression with elastic bandages limits swelling. Elevation above heart level reduces fluid accumulation.
Heat therapy becomes appropriate after the initial inflammatory phase (usually 48-72 hours post-injury) or for chronic muscle tension. Heat increases blood flow, relaxes tight muscles, and provides soothing comfort. Use heating pads, warm baths, or hot water bottles for 15-20 minutes as needed.
Over-the-counter pain relievers including NSAIDs (ibuprofen, naproxen) reduce both pain and inflammation, while acetaminophen addresses pain without anti-inflammatory effects. Use as directed and be aware of potential side effects, particularly with prolonged use.
Gentle stretching of tight, painful muscles can provide relief, but avoid aggressive stretching during acute injury phases. Focus on slow, sustained stretches held for 20-30 seconds without bouncing.
Movement and Exercise Modifications
While rest is appropriate immediately following injury, prolonged immobility delays recovery. Active recovery—light movement that doesn't exacerbate pain—promotes healing by increasing blood flow and preventing excessive stiffness.
For DOMS, light cardiovascular exercise like walking or easy cycling reduces soreness more effectively than complete rest. For chronic tension, regular movement breaks throughout the day prevent muscle stiffness. When returning to exercise after injury, gradual progression prevents re-injury—follow the 10% rule by increasing intensity or duration by no more than 10% weekly.
Manual Therapy and Bodywork
Various hands-on techniques provide muscle pain relief. Massage therapy reduces muscle tension, improves circulation, and promotes relaxation. Research shows massage effectively reduces DOMS and enhances recovery. Self-massage using foam rollers or massage balls offers convenient relief for tight muscles.
Physical therapy provides targeted treatment including manual therapy techniques, corrective exercises, and movement retraining. This is particularly valuable for chronic pain or recurring injuries where movement patterns need correction.
Myofascial release techniques target the fascia—connective tissue surrounding muscles—which can become restricted and painful. Trigger point therapy addresses specific tender points within muscles that refer pain to other areas.
Nutritional Support for Muscle Recovery
Proper nutrition accelerates muscle healing and reduces pain. Protein provides amino acids necessary for muscle repair—aim for 0.7-1 gram per pound of body weight daily, distributed across meals. Include high-quality sources like lean meats, fish, eggs, dairy, legumes, and protein supplements if needed.
Anti-inflammatory foods reduce pain-promoting inflammation. Fatty fish rich in omega-3s (salmon, mackerel, sardines), colorful fruits and vegetables high in antioxidants, herbs and spices like turmeric and ginger, extra virgin olive oil, and nuts and seeds all combat inflammation naturally.
Hydration is critical—dehydration exacerbates muscle pain and cramping. Drink at least half your body weight in ounces daily, more if you're active or in hot environments. Include electrolyte-rich beverages when sweating heavily.
Address nutritional deficiencies that contribute to muscle pain. Have your vitamin D levels checked and supplement if low (many people need 2,000-5,000 IU daily). Ensure adequate magnesium intake through foods like leafy greens, nuts, seeds, and whole grains, or consider supplementation (300-500mg daily). Maintain potassium levels through fruits, vegetables, and legumes.
Supplements for Muscle Health and Pain Relief
Certain supplements have evidence supporting their use for muscle pain and recovery. Omega-3 fatty acids from fish oil reduce inflammation and may decrease exercise-induced muscle damage. Aim for 2-3 grams combined EPA and DHA daily.
Branched-chain amino acids (BCAAs) may reduce muscle soreness and damage when taken around workouts, particularly when training in a fasted state or during periods of high training volume.
Tart cherry juice and extract contain anthocyanins with anti-inflammatory properties. Studies show tart cherry reduces muscle soreness and accelerates recovery following intense exercise.
Turmeric and its active compound curcumin possess potent anti-inflammatory effects. Look for supplements with enhanced absorption (paired with black pepper extract) and follow dosing recommendations.
Magnesium supplementation helps those with deficiency or frequent muscle cramps. Magnesium glycinate is well-absorbed and less likely to cause digestive issues.
Greens and superfood supplements provide concentrated antioxidants and micronutrients that support overall recovery and reduce oxidative stress contributing to muscle damage.
Stress Management and Relaxation
Since stress contributes significantly to muscle tension and pain, stress management techniques provide substantial relief. Progressive muscle relaxation involves systematically tensing and releasing muscle groups to reduce overall tension. Meditation and mindfulness practices calm the nervous system and reduce pain perception.
Deep breathing exercises activate the parasympathetic nervous system, promoting relaxation. Yoga combines movement, stretching, and breath work to address both physical tension and psychological stress. Regular practice can significantly reduce chronic muscle pain.
Sleep Optimization
Quality sleep is essential for muscle recovery and pain management. During sleep, your body releases growth hormone, repairs tissues, and processes inflammation. Sleep deprivation increases pain sensitivity and impairs recovery.
Optimize sleep by maintaining consistent sleep-wake times, creating a cool, dark, quiet sleep environment, limiting screens before bed, avoiding caffeine in the afternoon and evening, and considering magnesium supplementation or other sleep-supporting nutrients if you struggle with sleep quality.
Ergonomic Improvements
For pain related to posture or repetitive movements, ergonomic modifications can be transformative. Ensure your workspace promotes neutral posture with monitor at eye level, chair supporting natural spinal curves, keyboard and mouse positioned to avoid shoulder strain, and frequent position changes throughout the day.
Use proper lifting technique (bend at knees, keep load close to body, avoid twisting), take regular breaks from repetitive activities, and invest in supportive mattresses and pillows that maintain spinal alignment during sleep.
Temperature Therapy Variations
Beyond basic ice and heat, consider contrast therapy—alternating hot and cold applications to increase circulation and reduce inflammation. Some athletes find cold water immersion or cryotherapy helpful for recovery, though evidence is mixed. Hot tubs and saunas provide relaxing heat therapy that eases muscle tension.
Topical Treatments
Topical analgesics containing menthol, camphor, or capsaicin provide localized pain relief by creating counter-irritant sensations that distract from pain signals. Magnesium oil or gel applied topically may help muscle soreness and cramps. CBD-containing topicals show promise for pain relief, though more research is needed.
Prevention: Stopping Muscle Pain Before It Starts
Preventing muscle pain is more effective than treating it. Implementing these strategies reduces your risk of developing problematic muscle discomfort.
Proper Training Principles
When exercising, follow progressive overload—gradually increase training demands rather than making sudden jumps. Include adequate warm-up to prepare muscles for activity and cool-down to aid recovery. Incorporate variety in your training to avoid overuse of specific muscle groups. Schedule regular recovery days when muscles can repair and adapt.
Movement Quality Over Quantity
Focus on proper form and technique in all activities—exercise, work movements, and daily tasks. Poor movement patterns create stress on muscles leading to pain and injury. Consider working with fitness professionals or physical therapists to ensure optimal movement quality.
Balanced Strength and Flexibility
Develop balanced strength across opposing muscle groups to prevent imbalances that lead to pain. Combine resistance training with regular flexibility work. Both strong and flexible muscles are less prone to injury and pain.
Lifestyle Factors
Maintain healthy body weight to reduce stress on muscles and joints. Stay consistently hydrated rather than trying to catch up when thirsty. Manage stress through regular relaxation practices before tension becomes chronic. Prioritize sleep as non-negotiable recovery time.
Listen to Your Body
Develop body awareness to recognize early warning signs of overuse or developing problems. Mild muscle fatigue is normal; sharp pain or pain that persists multiple days deserves attention. Address minor issues before they become major problems.
When to Seek Professional Help
While many cases of muscle pain respond to self-care, certain situations require medical evaluation and professional treatment.
Medical Evaluation Indicators
Seek medical care if pain is severe or debilitating, persists beyond two weeks without improvement, is accompanied by systemic symptoms like fever or unexplained weight loss, includes significant weakness that interferes with function, or occurs following significant trauma. Additionally, if you have underlying health conditions (diabetes, vascular disease, autoimmune conditions) or take medications that might cause muscle problems, discuss persistent muscle pain with your healthcare provider.
Healthcare Professionals Who Can Help
Your primary care physician can evaluate muscle pain, order diagnostic tests, and provide initial treatment or referrals. Physical therapists specialize in movement-related pain and can design rehabilitation programs. Sports medicine specialists focus on activity-related injuries and performance optimization. Rheumatologists address inflammatory and autoimmune causes of muscle pain. Pain management specialists offer comprehensive approaches for chronic muscle pain conditions.
Diagnostic Tests
Depending on your symptoms and examination findings, your doctor may order blood tests to check for inflammatory markers, vitamin deficiencies, or muscle enzyme levels; imaging studies like X-rays, MRI, or ultrasound to visualize tissues; electromyography (EMG) to assess muscle and nerve function; or other specialized tests based on suspected conditions.
Living with Chronic Muscle Pain
For those dealing with chronic conditions causing persistent muscle pain, developing effective management strategies improves quality of life.
Acceptance and Adaptation
Chronic pain requires accepting limitations while focusing on what you can control. This doesn't mean giving up—it means finding sustainable ways to live well despite pain. Work with healthcare providers to develop comprehensive management plans addressing physical, psychological, and social aspects of chronic pain.
Pacing and Energy Conservation
Learn to pace activities to avoid boom-bust cycles where overdoing it leads to severe pain flares. Break tasks into smaller segments with rest periods. Prioritize important activities and delegate or eliminate less essential ones.
Multidisciplinary Approaches
Chronic muscle pain often responds best to multifaceted treatment combining medication when appropriate, physical therapy and exercise, psychological support addressing pain's emotional impact, nutritional optimization, stress management, and complementary therapies like acupuncture or massage.
Building Support Networks
Connect with others managing similar conditions through support groups (in-person or online). Don't underestimate the value of understanding from those who truly "get it." Work on communication with family, friends, and employers about your needs and limitations.
Reclaim Your Comfort and Mobility
Muscle pain doesn't have to control your life. By understanding its causes, recognizing concerning symptoms, and implementing evidence-based solutions, you can effectively manage discomfort and support your body's natural healing processes. Whether addressing acute soreness from a new workout or managing chronic pain conditions, the right combination of self-care strategies, nutritional support, and when necessary, professional intervention can make a significant difference.
Remember that muscles are remarkably resilient. With proper care, adequate recovery time, and attention to underlying causes, most muscle pain resolves completely. For chronic conditions, effective management strategies allow you to maintain activity and quality of life despite ongoing challenges.
Support Your Recovery Journey
Optimizing muscle recovery and managing pain effectively requires comprehensive nutritional support. Whether you need intra-workout supplementation to prevent exercise-induced damage, targeted sports care products for recovery and pain management, or nutrient-dense greens and superfoods to support overall healing and reduce inflammation, quality supplementation can enhance your body's natural repair processes.
Discover evidence-based products designed to support muscle health and recovery:
- Intra-Workout Supplements to fuel your training and minimize muscle damage
- Sports Care Products for comprehensive recovery and injury support
- Greens & Superfoods to provide anti-inflammatory nutrients and support healing
Don't let muscle pain hold you back. Give your body the support it needs to recover and thrive.
Disclaimer: This article is intended for informational and educational purposes only and should not be construed as medical advice, diagnosis, or treatment recommendations. The information provided about muscle pain, its causes, symptoms, and potential solutions is based on general health principles and available research, but individual circumstances vary significantly based on underlying health conditions, medications, age, fitness level, and other factors. Muscle pain can result from numerous causes ranging from benign exercise-induced soreness to serious medical conditions requiring immediate attention. Always consult with qualified healthcare professionals, including your physician, physical therapist, or sports medicine specialist, before starting any new treatment regimen, supplement protocol, or exercise program, particularly if you experience persistent, severe, or unusual muscle pain; have underlying medical conditions such as cardiovascular disease, diabetes, autoimmune disorders, or metabolic conditions; take prescription medications that may affect muscles; are pregnant or breastfeeding; or have a history of muscle, tendon, or joint injuries. The statements about supplements, natural remedies, and their effects have not been evaluated by the Food and Drug Administration, and products mentioned are not intended to diagnose, treat, cure, or prevent any disease. Supplements can interact with medications and may not be appropriate for everyone. This article should not delay appropriate medical evaluation—serious conditions including rhabdomyolysis, compartment syndrome, infections, blood clots, and others can present with muscle pain and require urgent medical treatment. If you experience severe pain, significant weakness, muscle pain accompanied by fever, dark urine, chest pain, difficulty breathing, or sudden severe pain without clear cause, seek immediate medical attention. This article cannot replace personalized medical evaluation and treatment from healthcare professionals who can assess your specific situation and provide recommendations tailored to your individual health profile and needs.
Share