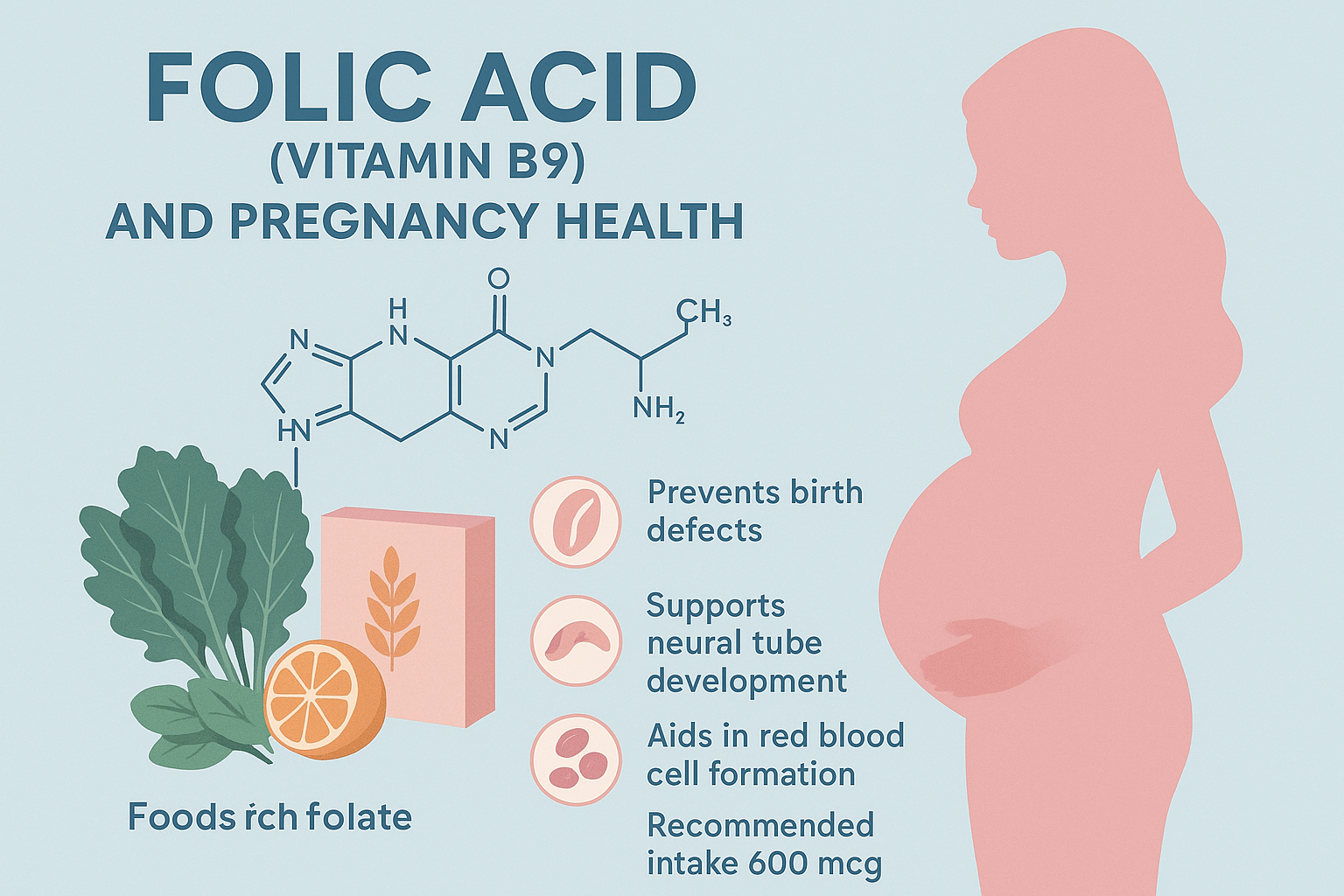
The Role of Folic Acid (Vitamin B9) in Pregnancy Health
The Vitamin That Prevents Birth Defects
In the 1990s, a medical breakthrough changed pregnancy outcomes forever. Researchers definitively proved that adequate folic acid intake before and during early pregnancy could prevent up to 70% of neural tube defects—devastating birth defects affecting the brain and spine. This discovery was so significant that the U.S. and many other countries mandated folic acid fortification of grain products, leading to a dramatic 35% reduction in neural tube defects.
Despite this success, neural tube defects still affect approximately 3,000 pregnancies annually in the United States alone. Many of these cases could be prevented with one simple intervention: adequate folic acid intake beginning before conception.
The challenge is timing. The neural tube—which develops into the baby's brain and spinal cord—closes within the first 28 days of pregnancy, often before a woman even knows she's pregnant. By the time pregnancy is confirmed, the critical window for preventing neural tube defects has often passed.
This is why understanding folic acid isn't just important for pregnant women—it's essential for every woman of reproductive age. Whether you're actively trying to conceive, might become pregnant, or simply want to understand this vital nutrient, this comprehensive guide provides the knowledge you need to protect maternal and fetal health.
What Is Folic Acid and Why Is It Different from Folate?
The terms "folic acid," "folate," and "vitamin B9" are often used interchangeably, but understanding the distinctions matters for optimal health.
Folate: The Natural Form
Folate is the naturally occurring form of vitamin B9 found in foods. It's actually a family of compounds called folates (plural) that exist in various forms in plant and animal foods. Natural folates are bioavailable but can be destroyed by heat, light, and food processing.
Food sources: Leafy greens, legumes, citrus fruits, asparagus, Brussels sprouts, and fortified foods.
Folic Acid: The Synthetic Form
Folic acid is the synthetic, oxidized form of vitamin B9 used in supplements and food fortification. It's more stable than natural folate, surviving cooking and storage better, which is why it's used for fortification.
However, folic acid must be converted by your body into the active forms—primarily 5-methyltetrahydrofolate (5-MTHF)—before it can be used. This conversion process requires several enzymatic steps, and genetic variations can affect how efficiently your body performs these conversions.
5-MTHF: The Active Form
5-MTHF (also called methylfolate or levomefolate) is the biologically active form that your body uses directly. It's what folic acid eventually becomes after conversion. Some supplements now provide 5-MTHF directly, bypassing the need for conversion.
Why This Matters
For most people, folic acid works perfectly well—their bodies efficiently convert it to active forms. However, approximately 40-60% of the population has genetic variations in the MTHFR (methylenetetrahydrofolate reductase) gene that reduce their ability to convert folic acid to 5-MTHF. For these individuals, taking 5-MTHF supplements may be more effective.
The practical takeaway: Whether you take folic acid or 5-MTHF, ensuring adequate vitamin B9 status before and during pregnancy is what matters most.
How Folic Acid Supports Pregnancy Health
1. Neural Tube Defect Prevention: The Primary Benefit
The Critical Window
The neural tube forms and closes between days 21-28 after conception (approximately weeks 5-6 of pregnancy when counting from the last menstrual period). This structure will develop into the baby's brain, spine, and spinal cord. If the neural tube doesn't close properly, serious birth defects result:
Spina bifida: The spinal column doesn't close completely, potentially causing paralysis, loss of bladder and bowel control, and learning disabilities. Severity ranges from mild (requiring minor treatment) to severe (requiring multiple surgeries and lifelong care).
Anencephaly: Most or all of the brain fails to develop. This condition is always fatal, either before or shortly after birth.
Encephalocele: Brain tissue protrudes through an opening in the skull, causing varying degrees of developmental delays and physical disabilities.
The Evidence
Landmark studies in the 1980s and 1990s demonstrated that folic acid supplementation reduces neural tube defect risk by 50-70%. Research shows:
- Women taking 400mcg of folic acid daily before conception reduced neural tube defect risk by 50%
- Higher doses (4,000mcg) for women with previous affected pregnancies reduced recurrence risk by 72%
- Mandatory folic acid fortification programs reduced neural tube defect rates by 19-55% in various countries
How It Works
Folic acid supports the rapid cell division required for neural tube closure. It's essential for DNA synthesis, cell division, and proper gene expression. Without adequate folate, cells cannot divide properly, and the neural tube fails to close correctly. The neural tube cells are among the fastest-dividing in early pregnancy, making them particularly vulnerable to folate deficiency.
2. DNA Synthesis and Cell Division
Pregnancy requires extraordinary cell division—a single fertilized egg becomes 37 trillion cells by birth. Folic acid is absolutely essential for this process because it:
- Provides single-carbon units needed to synthesize nucleotides (DNA building blocks)
- Supports the methylation processes that regulate gene expression
- Enables proper chromosome replication and segregation during cell division
- Prevents DNA damage and mutations
Without adequate folate, cells cannot replicate their DNA efficiently, leading to impaired growth and development.
3. Placental Development and Function
The placenta is the life-support system connecting mother and baby, delivering nutrients and oxygen while removing waste. Folic acid supports:
- Proper placental formation and growth
- Healthy blood vessel development within the placenta
- Efficient nutrient transfer to the developing baby
- Prevention of placental complications like preeclampsia
Research shows that folate deficiency is associated with placental abnormalities, which can lead to pregnancy complications including preterm birth, low birth weight, and preeclampsia.
4. Prevention of Other Birth Defects
While neural tube defects receive the most attention, adequate folic acid may reduce risks of other congenital abnormalities:
Congenital heart defects: Some studies suggest folic acid supplementation reduces certain heart defect risks by 15-30%, though evidence is mixed.
Orofacial clefts: Research indicates modest reductions in cleft lip and palate risk, though not as dramatically as for neural tube defects.
Limb defects: Limited evidence suggests potential protective effects for certain limb malformations.
Urinary tract abnormalities: Some studies show reduced risk of urinary system birth defects.
5. Prevention of Pregnancy Complications
Beyond birth defects, adequate folic acid status may reduce risks of:
Preterm birth: Some studies link low folate status with increased preterm delivery risk Low birth weight: Folate deficiency may impair fetal growth Preeclampsia: A dangerous condition involving high blood pressure and organ damage; some research suggests folate may offer modest protective effects Pregnancy loss: While evidence is inconsistent, some studies suggest adequate folate may reduce miscarriage risk
6. Maternal Health Support
Folic acid benefits maternal health during pregnancy:
Prevents megaloblastic anemia: A type of anemia where red blood cells become abnormally large and dysfunctional. Pregnancy increases folate demands, making deficiency more likely without supplementation.
Supports increased blood volume: Blood volume expands by 40-50% during pregnancy, requiring increased red blood cell production that depends on adequate folate.
Supports mood and mental health: Folate is essential for neurotransmitter production. Some research links adequate folate status with reduced depression risk during pregnancy and postpartum.
Reduces homocysteine levels: Elevated homocysteine (an amino acid) is associated with cardiovascular complications and pregnancy issues. Folate helps convert homocysteine to beneficial compounds.
7. Long-term Child Development
Emerging research suggests maternal folate status may influence:
Cognitive development: Some studies show associations between adequate maternal folate and better cognitive outcomes in children Behavioral outcomes: Research exploring links between maternal folate and reduced autism risk shows mixed results; more research is needed Metabolic programming: Maternal nutrition, including folate, may influence the child's lifelong disease susceptibility through epigenetic mechanisms
How Much Folic Acid Do You Need?
Recommended Dosages by Stage
Women of Reproductive Age (Pre-Conception)
- 400-800mcg daily: All women capable of becoming pregnant should take this amount, whether actively trying to conceive or not, because approximately half of pregnancies are unplanned and neural tube closure occurs before most women know they're pregnant.
During Pregnancy (All Trimesters)
- 600-800mcg daily: This increased amount supports the demands of fetal development and maternal physiological changes.
Breastfeeding
- 500mcg daily: Folate passes into breast milk, and maternal stores need replenishment.
Higher-Risk Women Women with the following risk factors need higher doses under medical supervision:
- 4,000mcg (4mg) daily: Women who previously had a pregnancy affected by neural tube defects
-
Higher doses may be considered for:
- Women with diabetes (type 1 or type 2)
- Women taking anti-seizure medications (particularly valproic acid or carbamazepine)
- Women with obesity (BMI ≥30)
- Women with MTHFR gene variants (may benefit from methylfolate instead)
- Women with celiac disease or other malabsorption disorders
- Multiple pregnancy (twins, triplets, etc.)
Upper Limit The tolerable upper intake level is 1,000mcg daily from supplements and fortified foods for the general population. Higher amounts should only be taken under medical supervision because excessive folic acid may mask vitamin B12 deficiency symptoms or potentially have other adverse effects.
Best Food Sources of Folate
While supplementation is recommended, folate-rich foods provide additional benefits through their complete nutrient packages:
Leafy Green Vegetables (per cooked cup):
- Spinach: 263mcg (66% DV)
- Turnip greens: 170mcg (42% DV)
- Collard greens: 177mcg (44% DV)
- Mustard greens: 103mcg (26% DV)
- Romaine lettuce: 76mcg (19% DV)
Legumes (per cooked cup):
- Lentils: 358mcg (90% DV)
- Black beans: 256mcg (64% DV)
- Pinto beans: 294mcg (74% DV)
- Chickpeas: 282mcg (71% DV)
- Lima beans: 156mcg (39% DV)
Vegetables:
- Asparagus (4 spears): 89mcg (22% DV)
- Brussels sprouts (1/2 cup): 78mcg (20% DV)
- Broccoli (1/2 cup): 52mcg (13% DV)
- Avocado (1/2 fruit): 82mcg (21% DV)
Fruits:
- Orange (1 large): 55mcg (14% DV)
- Papaya (1 cup): 53mcg (13% DV)
- Banana (1 medium): 24mcg (6% DV)
- Strawberries (1 cup): 40mcg (10% DV)
Fortified Foods:
- Fortified cereal (varies): 100-400mcg per serving
- Enriched bread (1 slice): 43mcg (11% DV)
- Enriched pasta (1 cup cooked): 102mcg (26% DV)
- Enriched rice (1 cup cooked): 153mcg (38% DV)
Other Sources:
- Beef liver (3 oz): 215mcg (54% DV)
- Eggs (1 large): 22mcg (6% DV)
- Sunflower seeds (1/4 cup): 82mcg (21% DV)
Important Notes:
- Folate in food is less bioavailable than folic acid in supplements (about 50-60% as available)
- Cooking destroys some folate—steaming is better than boiling
- Even folate-rich diets typically don't provide the 400-800mcg recommended for pregnancy prevention
- This is why supplementation is recommended regardless of diet quality
When to Start Taking Folic Acid
The Critical Message: Start Before Pregnancy
The most important fact about folic acid supplementation is that it must begin before conception. Here's why:
- Neural tube closure occurs at days 21-28 post-conception (weeks 5-6 of pregnancy)
- Most women don't know they're pregnant until week 4-6 (two or more weeks after a missed period)
- Building adequate folate stores takes several weeks to months
- By the time pregnancy is confirmed, the window for neural tube defect prevention has often closed
Recommended Timeline:
At least 1-3 months before trying to conceive: Begin taking 400-800mcg daily. This ensures adequate tissue levels when conception occurs.
Throughout pregnancy: Continue supplementation through all three trimesters to support ongoing fetal development and maternal needs.
During breastfeeding: Continue with 500mcg daily to support milk production and maternal recovery.
For all women of reproductive age: Since approximately 50% of pregnancies are unplanned, health organizations recommend that all women capable of becoming pregnant take 400mcg daily, regardless of whether they're actively trying to conceive.
Choosing the Right Folic Acid Supplement
Standard Folic Acid vs. Methylfolate (5-MTHF)
Standard Folic Acid:
- Pros: Extensively studied, proven effective, widely available, inexpensive, used in all major neural tube defect prevention trials
- Cons: Requires enzymatic conversion to active forms; may be less effective for women with MTHFR variants; high doses might lead to unmetabolized folic acid in blood
Methylfolate (5-MTHF):
- Pros: Already in active form, bypasses conversion step, may be more effective for MTHFR variants, no unmetabolized folic acid, better absorbed in some people
- Cons: More expensive, less long-term research than folic acid (though existing research is positive), not all prenatal vitamins contain it
Who Should Consider Methylfolate:
- Women with known MTHFR gene variants (particularly C677T homozygous)
- Women who haven't responded well to standard folic acid
- Those with digestive issues affecting nutrient absorption
- Women with a family history of MTHFR-related issues
- Those who prefer the active form as a precautionary measure
Bottom Line: Both forms are effective. Standard folic acid has the strongest evidence base and works well for most women. Methylfolate may offer advantages for certain individuals but is more expensive. Either form is vastly better than no supplementation.
Prenatal Vitamins vs. Standalone Folic Acid
Prenatal Vitamin Formulas: Most comprehensive option providing folic acid plus other essential pregnancy nutrients:
- Iron (prevents anemia)
- Calcium (supports bone development)
- Vitamin D (supports calcium absorption and immune function)
- DHA (supports brain development)
- Iodine (supports thyroid and brain development)
- Vitamin B12 (works synergistically with folate)
- Other B vitamins, zinc, and essential nutrients
Standalone Folic Acid: Appropriate when:
- You already eat a nutrient-rich diet and only need folic acid supplementation
- You take separate supplements for other nutrients
- You have difficulty tolerating prenatal vitamins
- You're in the pre-conception phase and want to start folic acid before investing in full prenatal vitamins
Recommendation: Most healthcare providers recommend comprehensive prenatal vitamins starting at least 1-3 months before conception and continuing throughout pregnancy and breastfeeding.
What to Look For in Supplements
- Amount: 400-800mcg of folic acid or methylfolate (check label)
- Form: Either folic acid or 5-MTHF/methylfolate
- Third-party testing: Look for USP, NSF, or ConsumerLab verification
- Expiration date: Folic acid degrades over time; don't use expired supplements
- Other B vitamins: B12, B6, and other B vitamins work synergistically with folate
- Avoid mega-doses: Unless medically indicated, stay under 1,000mcg daily
- Check for allergens: If you have sensitivities to gluten, dairy, etc.
Special Considerations and Risk Factors
MTHFR Gene Variants
MTHFR (methylenetetrahydrofolate reductase) is an enzyme that converts folic acid to its active form. Common genetic variants reduce enzyme activity:
C677T variant:
- Heterozygous (one copy): 30-40% reduced enzyme activity
- Homozygous (two copies): 70% reduced enzyme activity
A1298C variant:
- Generally less impact than C677T
- Compound heterozygous (one of each variant): Moderate impact
Implications: Women with MTHFR variants may have elevated homocysteine levels and may benefit from methylfolate supplementation instead of folic acid. However, most women with MTHFR variants respond adequately to standard folic acid doses. Higher doses or methylfolate forms may be recommended if standard supplementation doesn't normalize homocysteine levels.
Should you get tested? MTHFR testing isn't routinely recommended. If you have a history of recurrent pregnancy loss, family history of neural tube defects, personal history of blood clots, or elevated homocysteine, discuss testing with your healthcare provider.
Medications That Interfere with Folate
Several medications increase folate needs:
Anti-seizure medications: Phenytoin, carbamazepine, valproic acid (women taking these need 4,000-5,000mcg daily) Methotrexate: Used for autoimmune diseases and cancer (interferes with folate metabolism) Sulfasalazine: Used for inflammatory bowel disease Metformin: Diabetes medication may reduce folate absorption Certain antibiotics: Trimethoprim interferes with folate metabolism
If you take any of these medications, discuss higher folic acid doses with your healthcare provider before conception.
Medical Conditions Affecting Folate Status
Celiac disease and inflammatory bowel disease: Impaired nutrient absorption may require higher doses Kidney disease: Especially if on dialysis, which removes folate Liver disease: Impaired folate metabolism may require modified supplementation Sickle cell disease: Higher folate needs due to increased red blood cell production Thalassemia: Similar to sickle cell disease
Obesity and Folic Acid
Research suggests women with obesity (BMI ≥30) may need higher folic acid doses because:
- Fat tissue may sequester folate
- Obesity is associated with chronic inflammation that increases folate needs
- Risk of neural tube defects is higher in obese women despite similar folic acid intake
Some experts recommend 800-1,000mcg daily for women with obesity, though official guidelines don't differ by weight.
Can You Take Too Much Folic Acid?
While folic acid is water-soluble (excess is generally excreted), concerns exist about very high intakes:
Masking B12 Deficiency: High folic acid intake can correct the anemia of B12 deficiency without addressing the underlying deficiency, allowing neurological damage to progress. This is why prenatal vitamins should include B12.
Unmetabolized Folic Acid: Very high doses (above 1,000mcg) may lead to unmetabolized folic acid circulating in blood. Health implications are unclear but being researched.
Potential Cancer Concerns: Very high doses might promote growth of existing precancerous cells (though evidence is limited and inconsistent). Standard prenatal doses (400-800mcg) have not shown increased cancer risk.
Interference with Immune Function: Some research suggests very high doses might affect natural killer cell activity, though evidence is preliminary.
Bottom Line: The 400-800mcg recommended for pregnancy is both safe and effective. Don't exceed 1,000mcg daily without medical supervision. More is not necessarily better.
Beyond Supplements: A Folate-Rich Lifestyle
Supplements are essential, but a folate-rich lifestyle provides comprehensive benefits:
Dietary Strategies:
- Eat leafy greens daily (spinach, kale, collards)
- Include legumes regularly (lentils, beans, chickpeas)
- Snack on oranges and fortified foods
- Steam or lightly cook vegetables to preserve folate
- Include folate-rich foods throughout the day, not just one meal
Other Healthy Pregnancy Practices:
- Avoid alcohol completely (interferes with folate metabolism and causes birth defects)
- Don't smoke (impairs nutrient absorption and harms fetal development)
- Maintain healthy weight before conception
- Manage chronic health conditions
- Take prescribed medications as directed
- Avoid harmful substances and unnecessary medications
- Get regular prenatal care
Take Control of Your Pregnancy Health
Folic acid supplementation is one of the simplest, most effective interventions in all of medicine. For less than a dollar per month, you can dramatically reduce your baby's risk of devastating birth defects that cause lifelong disability or death.
The science is clear, the evidence is overwhelming, and the recommendation is simple: Every woman capable of becoming pregnant should take 400-800mcg of folic acid daily, starting before conception and continuing throughout pregnancy.
Don't wait until you're pregnant to start. Don't assume your diet provides enough. Don't skip days thinking it doesn't matter. The neural tube closes in the first month of pregnancy, often before you know you're expecting. By then, it may be too late to prevent defects that adequate folate could have stopped.
Protect your future baby by starting folic acid supplementation today.
Ready to support your pregnancy health with high-quality prenatal vitamins and women's health supplements? Explore comprehensive formulations designed for preconception, pregnancy, and postpartum at Matevara's Women's Health Collection. Discover prenatal vitamins with optimal folic acid or methylfolate levels, plus essential nutrients for maternal and fetal health.
Your baby's healthy development starts before conception. Make folic acid part of your daily routine now.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider for personalized guidance regarding prenatal vitamins, folic acid supplementation, and pregnancy health. Recommended dosages may vary based on individual medical history, risk factors, and health conditions. If you have previously had a pregnancy affected by neural tube defects or have specific risk factors, discuss higher supplementation doses with your healthcare provider. Never exceed recommended doses without medical supervision.
Share